Spermogram
The spermogram represents the developed analysis of an ejaculate (sperm), a sperm research under a microscope. This analysis allows to estimate fertility of the man, that is his ability to conceive. Deviations of indicators of a spermogram from norm demonstrate decrease in a possibility of conception in the natural way. However similar deviations do not exclude probability of conception. Lead change of morphology of spermatozoa, physical and chemical properties of an ejaculate, existence of foreign components in sperm to decrease in fertility.
Preparation for a spermogram
In three-five days prior to a research it is necessary to exclude alcohol intake, medicines, especially antibiotics. It is forbidden to visit a bath and a sauna as the overheat of spermatozoa will lead to their death. Before a research it is necessary to avoid excessive nervousness and stresses. For this span sexual abstinence is obligatory.
Masturbation is considered the main way of receiving an ejaculate for a spermogram. By preparation for a research collect all sperm which was emitted at an ejaculation. Sperm for a spermogram (with the very first and latest portion) is collected in a plastic sterile container. Reliability of results of a research of sperm directly depends on transportation conditions, and also on time through which the container was brought to laboratory. It is preferable that the container was delivered within twenty minutes after an ejaculation. It is not necessary to receive for a spermogram sperm by means of the interrupted sexual intercourse, oral sexual intercourse, sexual intercourse in condom. Saliva, condom latex components, vulval allocations can negatively affect quality of an ejaculate. It is necessary for obtaining reliable and objective result that the spermogram was executed four times with a break in two weeks.
Norms for a spermogram
For a spermogram the following values of the main indicators are considered as norms:
- semen volume (to 4 ml);
- viscosity of sperm (to 0,5 cm);
- concentration of spermatozoa (more than 20 million in 1 ml of semen);
- quantity of spermatozoa (more than 60 million in semen);
- mobility of spermatozoa (And> 25% or A+B> 50%);
- morphology of spermatozoa (more than 20%);
- quantity of live spermatozoa (more than 50%);
- quantity of cells of a spermatogenesis (to 2%).
Interpretation of a spermogram
At a research, first of all, check sperm fluidifying time. At increase in time of fluidifying spermatozoa gain the full-fledged mobility longer. At very liquid semen the probability of fertilization considerably decreases. Viscosity of sperm is determined by length of the thread formed by sperm at running off from a special needle or a pipette. Increase in viscosity of an ejaculate is usually observed at a chronic inflammation of gonads – a vesiculitis or prostatitis.
Dense sperm on a spermogram testifies to possible male infertility. To define viscosity of sperm, she is brought together in the syringe and released through a special needle. Ejaculate volume is very important for the analysis. Optimum volume ejaculate volume to 4 ml is considered. The small volume of the emitted semen indicates very weak ability to fertilization and a problem with male health. Decrease in volume of semen demonstrates insufficient function of seed bubbles, a prostate. Exceeding of volume of an ejaculate can be connected with inflammatory process in gonads.
Normal color of sperm yellowish, white or grayish. Emergence of a brown or red shade of sperm happens at a chronic vesiculitis, a calculous form of prostatitis, injuries of generative organs. Sperm gains yellow color at the use of food dyes and some medicines.
Tells quantity of spermatozoa about a possibility of conception. It is possible to count quantity of spermatozoa by means of a special microscope. Normal quantity twenty million spermatozoa in one millimeter of an ejaculate are considered.
At interpretation of a spermogram special attention is paid by mobility of spermatozoa. The most mobile spermatozoa will connect to an ovum rather. The spermogram helps to define quantity of abnormal spermatozoa.
Disturbances of reproductive function are defined by means of acidity of semen. On a spermogram normal рН from 7,2 to 7,8 has to make sperms. The deviation рН from norm indicates a possible inflammation of gonads (a vesiculitis, prostatitis).
Reduction of quantity of spermatozoa on a spermogram is called an oligospermatism. The oligospermatism usually testifies to reduced overall performance of testicles. Work of testicles can be oppressed because of decrease in concentration in blood of male sex hormones, inflammatory process, the postponed toxic defeat of an epithelium of testicles, metabolism change. Polizoospermiya – the increased quantity of spermatozoa (more than 120 million/ml).
Mobility of spermatozoa – the most important indicator of a spermogram. On mobility spermatozoa can be divided into four groups:
- group A – active spermatozoa with the rectilinear movement;
- group B – slow-moving spermatozoa with the rectilinear movement;
- group C – slow-moving spermatozoa with rotary or oscillating motion;
- group D – motionless spermatozoa.
Astenozoospermiya – decrease in mobility of spermatozoa. Mobility of spermatozoa can decrease from various diseases and different thermal and toxic impacts on testicles.
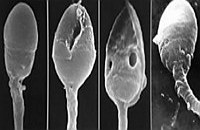
The morphology of spermatozoa is considered very important indicator of a spermogram. This indicator of a spermogram reflects percentage of spermatozoa, capable to fertilization. A necrospermia – decrease in concentration of live spermatozoa. Agglutination (pasting of spermatozoa) can be observed at chronic inflammatory processes in male gonads. At agglutination mobility of spermatozoa almost always decreases.
Assessment of results of a spermogram
 Interpretation of a spermogram is carried usually out by the andrologist. If at interpretation of a spermogram all indicators appear within norm, then chances of bystry and successful conception are rather high. If there are any deviations, then approximately in a month appoint a repeated research. As results of a spermogram can vary, final conclusions can be drawn only after two-three researches. It should be noted that only by results of a spermogram it is impossible to make accurately the diagnosis as the probability of conception depends on many other factors – reproductive health of the woman, frequency and duration of sexual intercourse, and also age and a condition of the patient.
Interpretation of a spermogram is carried usually out by the andrologist. If at interpretation of a spermogram all indicators appear within norm, then chances of bystry and successful conception are rather high. If there are any deviations, then approximately in a month appoint a repeated research. As results of a spermogram can vary, final conclusions can be drawn only after two-three researches. It should be noted that only by results of a spermogram it is impossible to make accurately the diagnosis as the probability of conception depends on many other factors – reproductive health of the woman, frequency and duration of sexual intercourse, and also age and a condition of the patient.
The most rare disease – a disease the Kura. Only representatives of the tribe Faure in New Guinea are ill it. The patient dies of laughter. It is considered that eating of a human brain is an origin of a disease.

Within several decades of our compatriots convinced that the use of butter nasty affects on...
Section: Articles about health
According to data of World Health Organization, the cataract is diagnosed almost for 7% of the population of Earth. The statistics of incidence is considered not full as at an initial stage the illness, as a rule, does not cause to the person of special inconveniences, and many having got sick...
Section: Articles about health
According to World Health Organization, every third inhabitant of Earth has excess weight, and every tenth has obesity. The reason of this phenomenon, according to specialists, roots in one not very comforting fact: most of people consume much more calories, than it is necessary. How it turns out what we overeat? Why it is so difficult to refuse an excess portion tasty or additives? Let's try to find out what factors prevent us to eat food with reasonable moderation....
Section: Articles about health
It is difficult to revaluate importance of kidneys for an organism. These bodies not only perform work on purification of blood of decomposition products and выв...
Section: Articles about health
Since the moment when the child becomes a school student, his sight begins to be exposed to the strengthened loadings which are supplemented with viewing of animated films and long computer games. During this period of life of the child development not completely created bodies to a zra...
Section: Articles about health
The phenomenon of improvement of a condition of the patients at administration of drugs who are not containing active agents, so-called effect of placebo is known long ago. At the end of the 18th century the American doctor Perkins began to treat people the "miracle" sticks made of alloy of steel and brass. Was for several minutes to press such subject enough to a sore point that it became much easier for the patient. Having suspected Perkins of charlatanism, his colleagues tried to repeat "miracle" by means of sticks, steles...
Section: Articles about health
Women quite often suffer from complexes concerning the sizes of the bust. Strangely enough, reason душевног...
Section: Articles about health
Smoking not only exerts a negative impact on the state of health of the consumer of tobacco products, but is an air polluter the substances potentially dangerous to people around. In recent years significantly the number of people, стремящ increased...
Section: Articles about health
Coffee - the tonic loved by many for the invigorating aroma and deep taste. Having the stimulating effect, coffee increases working capacity, promotes concentration of attention, fights against drowsiness and improves mood. Statistically, about 30% of inhabitants of the planet regularly use coffee, from them more than 8% are "coffee-achievers" - the persons using more than 3 cups of drink a day....
Section: Articles about health
The hysteromyoma is diagnosed more than at a third of women 35 years are more senior. This high-quality new growth, which on early a stage...
Section: Articles about health
The number of long-livers is very small. One person from 5 thousand lives up to age of 90 years, and the centenary boundary steps over only one of 20 thousand. However, doctors claim that each of us is quite able to affect own destiny. At the same time speech to Ida...
Section: Articles about health
Almost each of us during life faced dissatisfaction with own body. At such moments, as a rule, we begin to shame ourselves, urgently we go on the most rigid diet promising minus of 10 kg in a week, or we exhaust ourselves in the gym to almost death. As a rule, similar attempts come to an end with a campaign to the refrigerator for jamming of the next stress. Further history repeats itself with individual frequency....
Section: Articles about health
Visit of doctors – business not the most pleasant, and many people do not hurry to undergo necessary planned inspections. Such behavior...
Section: Articles about health
Statistically, at the address to doctors seven of each ten patients complain of a headache. Actually it is much more people who are periodically feeling unpleasant feelings such. Many people, apart from a headache the reason for serious fear...
Section: Articles about health
High temperature - a frequent symptom of such widespread diseases as a SARS, quinsy, pneumonia, etc. To reduce heat, having facilitated a condition of the patient, doctors recommend to accept antipyretics, however their use is not always possible. Too frequent use of these drugs can lead to allergic reactions, and also overdose, causing poisoning. It happens also that there are no antipyretics simply in the house. In these situations it is pertinent to use it...
Section: Articles about health
The list of stereotypes of which, apparently, all know strongly includes following: British surely eat for breakfast овсянк...
Section: Articles about health
The next flu epidemic leads to the next panic, from year to year we give in on these manipulations: professionally alarming voice of the announcer in news, reports with calculation of the died patients, an interview with people in white dressing gowns and advertizing of anti-influenza means ра...
Section: Articles about health
Olive oil – the product capable to make a powerful contribution to health of the person if it includes it in the diet. The rich vitamin composition of oil does it by a product number one from many diseases including from deadly. Only two tablespoons of oil from olives in day prevent emergence of diseases of vessels and heart, cancer, problems with digestion, presenilation, a depression and many other illnesses which treatment would demand a lot of time and forces. Let's consider on...
Section: Articles about health
The advantage of swimming for the person is so high that this sport is not only the most popular, but also is widely applied in copper...
Section: Slideshow
For the person who daily since morning gathers for work it is very important to wake up vigorous and ready by day of work. Actually, each of us experiences difficulties with this, at first sight, simple business from time to time. On a condition of an organism after ночн...
Section: Articles about health
There is a lot of fans of beer in our country. Statistically, on each average Russian (including women and children) in a year about 60 liters of this drink are consumed. It is not a lot of, as in the Czech Republic or Germany, but figure all the same impressive. There is nothing to rejoice here: despite assurances of producers that beer is absolutely harmless, effects of its active consumption cannot be considered positive in any way. Here only part of that negative impact, which popular нап...
Section: Articles about health
Beauty shop – the place which is associated only with positive emotions: joy, pleasure, relaxation. One...
Section: Articles about health
Partial and the more so full loss of hearing significantly reduces quality of life. Difficulties with communication lead to loneliness and isolation. The person who badly hears experiences difficulties with social and professional implementation, quite often has problems in...
Section: Articles about health
Coffee – favourite drink of many. For the last decades it more than once already declared very harmful, extremely useful and even necessary for normal life activity. In spite of the fact that this product became for us usual for a long time, there are many myths about properties of coffee and its impact on a human body. Readers can get acquainted with the most widespread of similar delusions today....
Section: Articles about health
According to doctors, more than a half of men of 25-50 years suffer from frustration of the urinogenital sphere, but sees a doctor from them меньшинс...
Section: Articles about health
There comes the season of issues. Many Russians already dream of outdoor recreation, trips, beautiful seaside beaches. At this time there is no wish to think of problems with health and other unpleasant things, however there are subjects which require attention. Summer...
Section: Articles about health
Dogrose – one of the most widespread adornment and medicinal plants growing practically in all territory of our country. To most of Russians it is a beautiful bush it is known, first of all, as a source of fruits, extremely vitamin-rich. However curative properties of a dogrose are not limited to it at all. About how still it is possible to use a plant in the medical purposes, we will tell today....
Section: Articles about health